Defined for the first time in 1994 by the World Health Organization (WHO), osteopenia refers to an early state of bone loss where a person’s bone mineral density (BMD)-a measurement that determines bone density and strength-is lower than normal peak BMD, but not low enough to be classified as osteoporosis.
A diagnosis of osteopenia means that there is a greater risk for developing osteoporosis later on, but not everyone diagnosed with osteopenia develops osteoporosis. As a result, the medical community does not view osteopenia as a disease, but as a potential marker for further bone loss and fracture.
What Causes Osteopenia?
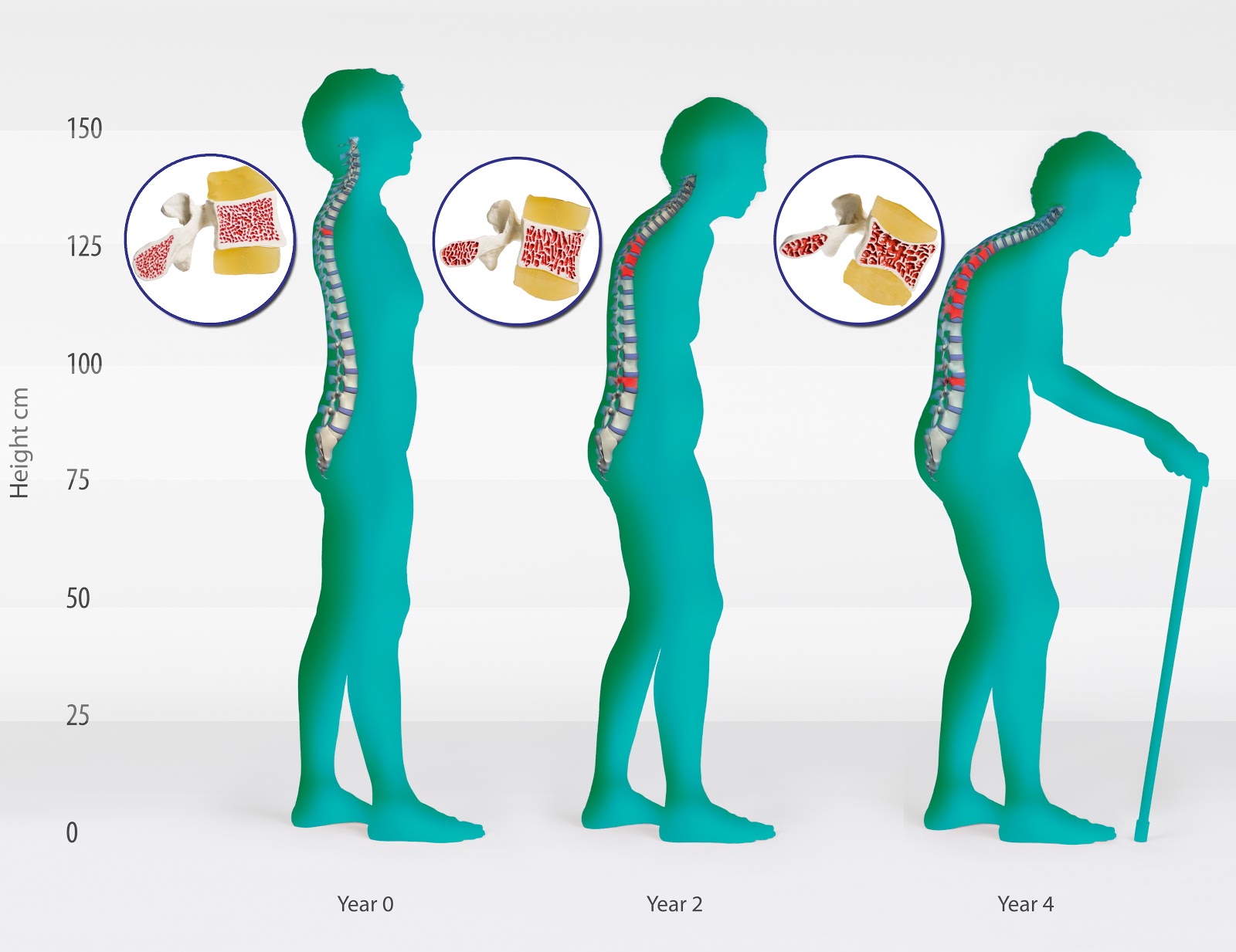
Several factors lead to a diagnosis of osteopenia, but it is important to note that both men and women naturally lose bone density as they age because the body reabsorbs bone cells faster than it can make new bone. This process makes bones weaker and more susceptible to fracture because it robs them of minerals, mass and structure. All people start losing bone mass after they reach peak bone mineral density at about age 30. The stronger and thicker your bones are by age 30, the better off your long-term prognosis is for healthy bones later in life.
That said, some people are more prone to osteopenia than others. Women are more likely than men to develop osteopenia because they have lower bone densities, and the loss of bone mass speeds up as women reach menopause and experience numerous hormonal changes. Moreover, some people diagnosed with osteopenia may not have bone loss-they may just naturally have a lower bone density.
Aside from the natural aging process and the subsequent loss of bone density, some factors can directly contribute to osteopenia:
- eating disorders or metabolism problems that rob the body of essential vitamins and minerals
- chemotherapy or medications such as steroids
- exposure to radiation
- family history of osteoporosis
- being white (Caucasian), or, to a lesser degree, being Asian
- being thin
- being bedridden or inactive for a long period of time
- smoking
- drinking excessively
- having a diet low in calcium and vitamin D
How is Osteopenia Diagnosed and Treated?
Osteopenia is diagnosed with the use of a bone mineral density test, typically a DEXA (dual-energy X-ray absorptiometry) scan. A diagnosis of osteopenia is confirmed when bone density measurements are between one standard deviation and two and a half standard deviations below the bone density of a normal young adult. The standard deviations for osteopenia are generally referred to as “T-scores” between -1 and -2.5. Osteoporosis is defined as a T-score below -2.5.
The World Health Organization recommends that women over the age of 65 and men over the age of 70 be screened for osteopenia and osteoporosis. Men and women who have more than one risk factor (e.g. an eating disorder or alcohol addiction) should be screened earlier.
While treating osteopenia with drugs like bisphosphonates remains controversial, people diagnosed with osteopenia can slow further bone loss with the following lifestyle changes:
- eating a diet rich in fruits, vegetables and calcium-enriched foods
- supplementing diet with calcium and vitamin D
- performing weigh-bearing exercises such as walking, hiking, jogging and resistance training
- quitting smoking
- avoiding excessive use of alcohol and cola
Whether you are over 30 or in your mid-60s, it is never too late to make lifestyle changes. A balanced diet and plenty of exercise today can mean slower bone loss tomorrow.