Recommendations on postmenopausal hormone therapy
February 27, 2007
The following Statement expresses the views of the International Menopause Society (IMS) on the principles of hormone therapy (HT) in the peri- and postmenopause period. Throughout the statement, the term HT will be used to cover all therapies including estrogens, progestogens, combined therapies and tibolone.
The previous IMS Statement in 2004 is still valid and serves as a basis for the current updated version.
We are aware of the geographical variations related to different priorities of medical care, different prevalence of diseases, and country-specific attitudes of the public, the medical community and the health authorities toward menopause management, which may all impact on hormone therapy. The following recommendations, therefore, give a global and simple overview that serves as a common platform on issues related to the various aspects of hormone treatment. This statement was reviewed and discussed by representatives of more than 60 National and Regional Menopause Societies from all continents. These recommendations can be easily adapted and modified according to local needs.
Governing Principles
Hormone therapy should be part of an overall strategy including lifestyle recommendations regarding diet, exercise, smoking and alcohol for maintaining the health of postmenopausal women. HT must be individualized and tailored according to symptoms and the need for prevention, as well as personal and family history, results of relevant investigations, the woman’s preferences and expectations. The risks and benefits of HT differ for women around the time of menopause compared to those for older women.
HT includes a wide range of hormonal products and routes of administration, with potentially different risks and benefits. Thus, the term ‘class effect’ is confusing and inappropriate.
Women experiencing a spontaneous or iatrogenic menopause before the age of 45 years and particularly before 40 are at higher risk for cardiovascular disease and osteoporosis. They will benefit from hormone replacement, which should be given at least until the normal age of menopause.
Counselling should convey the benefits and risks of HT in simple terms, e.g. absolute numbers rather than as percentage changes from baseline. This allows a woman and her physician to make a well-informed decision about HT.
HT should not be recommended without a clear indication for its use.
Women taking HT should have at least an annual consultation to include a physical examination, update of medical history, relevant laboratory and imaging investigations and a discussion on lifestyle.
There are no reasons to place mandatory limitations on the length of treatment.
Whether or not to continue therapy should be decided at the discretion of the well-informed hormone user and her health professional, dependent upon the specific goals and an objective estimation of benefits and risks.
Dosage should be titrated to the lowest effective dose. Lower doses of HT than have been used routinely can maintain quality of life in a large proportion of users. Long-term data on lower doses regarding fracture risk and cardiovascular implications are still lacking.
In general, progestogen should be added to systemic estrogen for all women with a uterus to prevent endometrial hyperplasia and cancer. However, progesterone and some progestins have specific beneficial effects that could justify their use besides the expected actions on the endometrium. Low-dose vaginal estrogens administered for the relief of urogenital atrophy do not require progestogen co-medication. Direct delivery of progestogen to the endometrial cavity from the vagina or by an intrauterine system is logical and may minimize systemic effects.
Androgen replacement should be reserved for women with clinical signs and symptoms of androgen insufficiency. In women with bilateral oophorectomy or adrenal failure, androgen replacement has significant beneficial effects, in particular on health-related quality of life and sexual function.
Benefits of Hormone Therapy
General
HT remains the most effective therapy for vasomotor and estrogen-deficient urogenital symptoms. Other menopause-related complaints, such as joint and muscle pains, mood swings, sleep disturbances and sexual dysfunction (including reduced libido) may improve during HT. Quality of life and sexuality are key factors to be considered in the management of the aging individual. The administration of individualized HT (including androgenic preparations when appropriate) improves both sexuality and overall quality of life.
Postmenopausal osteoporosis
HT is effective in preventing the bone loss associated with the menopause and decreases the incidence of all osteoporosis-related fractures, including vertebral and hip, even in patients at low risk. Although the magnitude of decline in bone turnover correlates with estrogen dosage, even lower than standard dose preparations maintain a positive influence on bone indices in most women. Based on updated evidence on effectiveness, cost and safety, HT is an appropriate first-line therapy in postmenopausal women presenting with an increased risk for fracture, particularly under the age of 60 years and for the prevention of bone loss in women with premature menopause. The protective effect of HT on bone mineral density declines after cessation of therapy at an unpredictable rate, although some degree of fracture protection may remain after cessation of HT.
The initiation of standard-dose HT is not recommended for the sole purpose of the prevention of fractures after the age of 60 years. Continuation of HT after the age of 60 years for the sole purpose of the prevention of fractures should take into account the possible long-term effects of the specific dose and method of administration of HT, compared to other proven therapies.
Regulatory Authorities should review their current recommendations as a priority.
Cardiovascular disease
Cardiovascular disease is the principal cause of morbidity and mortality in postmenopausal women. Major primary prevention measures (besides smoking cessation and diet control) are weight loss, blood pressure reduction, and diabetes and lipid control. There is evidence that HT may be cardioprotective if started around the time of menopause and continued long-term (often referred to as the ‘window of opportunity’ concept). HT reduces the risk of diabetes and has positive effects on other risk factors for cardiovascular disease such as the lipid profile and metabolic syndrome.
In women less than 60 years old, recently menopausal and without prevalent cardiovascular disease, the initiation of HT does not cause early harm and may reduce cardiovascular morbidity and mortality. Continuation of HT beyond the age of 60 should be decided as a part of the overall risk–benefit analysis.
Other benefits
HT has benefits for connective tissue, skin, joints and intervertebral disks. HT may reduce the risk of colon cancer. HT initiated around the time of menopause or by younger postmenopausal women is associated with a reduced risk of Alzheimer’s disease.
Potential Serious Adverse Effects of Hormone Therapy
Studies on the risks of postmenopausal hormone use have mainly focused on breast and endometrial cancer, venous thromboembolism (pulmonary embolism or deep vein thrombosis), stroke and coronary events.
Breast cancer
The incidence of breast cancer varies in different countries. Therefore, currently available data cannot necessarily be generalized. The degree of association between breast cancer and postmenopausal HT remains controversial.
Women should be reassured that the possible risk of breast cancer associated with HT is small (less than 0.1% per annum). For combined HT, observational data from the Million Women Study suggested that breast cancer risk was increased as early as the first year, raising serious reservations on possible methodologic flaws. On the contrary, randomized controlled data from the Women’s Health Initiative (WHI) study indicate that no increased risk is observed in women initiating HT, for up to 7 years. It should be noted that the majority of subjects in the WHI were overweight or obese.
Data from the WHI and Nurses’ Health Study suggest that long-term estrogen-only administration for 7 and 15 years, respectively, does not increase the risk of breast cancer in American women. Recent European observational studies suggest that risk may increase after 5 years.
There are insufficient data to evaluate the possible differences in the incidence of breast cancer using different types and routes of estrogen, progestin and androgen administration.
Baseline mammographic density correlates with breast cancer risk. This does not necessarily apply to the increase in mammographic density induced by HT.
The combined estrogen–progestogen therapy-related increase in mammographic density may impede the diagnostic interpretation of mammograms.
Endometrial cancer
Unopposed estrogen administration induces a dose-related stimulation of the endometrium. Women with a uterus should have progestogen supplementation.
Continuous combined estrogen–progestogen regimens are associated with a lower incidence of endometrial hyperplasia and cancer than occurs in the normal population.
Direct intrauterine delivery systems may have advantages. Regimens containing low-/ultra-low-dose estrogen and progestogen cause less endometrial stimulation and less bleeding.
Thromboembolism and cardiovascular events
The HT-related risk for serious venous thromboembolic events increases with obesity and thrombophilia. By avoiding first-pass hepatic metabolism, transdermal estrogen may avert the risk associated with oral HT. Late starters of standard-dose HT may have a transient slightly increased risk for coronary events. The risk of stroke is correlated with age. HT may increase the risk of ischemic stroke.
Safety data from studies of low-dose and ultra-low-dose regimens of estrogen and progestogen are encouraging.
Alternative Treatments
The efficacy and safety of complementary alternative medicines have not been demonstrated and further studies are required.
Selective serotonin reuptake inhibitors, selective noradrenaline reuptake inhibitors and gabapentin are effective in reducing vasomotor symptoms in short-term studies. Their long-term safety needs further evaluation.
There are no medical or scientific reasons to recommend unregistered ‘bioidentical hormones’. The measurement of hormone levels in the saliva is not clinically useful. These ‘customized’ hormonal preparations have not been tested in studies and their purity and risks are unknown.
Top Steroid Products Sales
CYX3 Oral Blend
|
Trenbolone 200
|
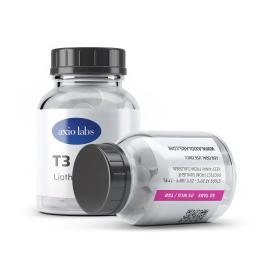
T3
|