About your bones
Bone is living tissue made up of specialised bone cells and, like the rest of the body, it is constantly being broken down and renewed. In childhood, more bone is made than is broken down, and bones therefore grow. Bone growth is nearly complete by the end of puberty, with only a small increase in bone strength occurring after the late teenage years.
From the mid 30s on there is a mismatch between bone production and bone breakdown. This results in a gradual decrease in bone strength with increasing age in both men and women. Bone needs exercise, just like muscle, to gain strength.
In addition, oestrogen has a fundamental role in maintaining bone strength in both men and women. The levels of oestrogen in the body fall at menopause and this speeds up the rate of loss of bone. During the first five years after menopause the average woman loses up to 10 percent of her total bone mass.
What is osteoporosis?
Osteoporosis occurs when bones lose their strength and density because of calcium loss, become fragile, and fracture (break) more easily. The word “osteoporosis” literally means bones with holes -brittle bones.
Osteoporosis particularly affects women in their middle and later years. (It is quite different from osteoarthritis which affects joint surfaces.)
Usually there is no sign that osteoporosis is developing until a fracture occurs. Breaks are most common in the spine, hip and wrist and often occur after only a minor fall. Osteoporotic fractures of the spine cause loss of height, pain and gradual development of the “dowager’s hump. This hump is caused by compression of the spinal fractures due to the force of gravity.
How common is osteoporosis?
More than one in every two women, and one in three men, will develop bone fractures due to osteoporosis. By the age of 70, more than one in five women will have been hospitalised with a fracture of the upper limb, spine or lower limb. Half of the people suffering hip fractures lose independence and require long-term nursing care. Osteoporosis costs Australia’s health care system $800 million per year.
Who is at risk?
The following factors all increase the risk of osteoporosis:
- a family history of osteoporosis (parent, sibling, grandparent);
- inadequate amounts of calcium in the diet;
- cigarette smoking;
- alcohol (more than 2 standard drinks per day for women);
- caffeine (more than 3 cups of tea or coffee per day);
- lack of exercise;
- early menopause, before the age of 45;
- having a thin, small body;
- prolonged absence of the menstrual period, which can occur as a result of excessive dieting or excessive exercise, and results in lowering oestrogen;
- long-term use of certain medications, such as corticosteroids for rheumatoid arthritis and asthma and thyroxine for an under active thyroid.
How can the risk be reduced?
Diet
Eat a healthy diet – plenty of fresh fruit, vegetables and whole grains. In particular, eat foods that are rich in calcium. Calcium is vital to build and maintain strong healthy bones, aid muscle function and aid function of the nervous system. The minimum recommended daily intake of dietary calcium is:
Category* |
Age (years) |
Calcium (mg) |
|
Children |
1-3 |
500 |
|
4-8 |
700 |
|
|
Girls |
9-11 |
1000 |
|
12-18 |
1300 |
|
|
Women |
19-50 |
1000 |
|
>50 |
1300 |
|
|
Pregnancy/Lactation: |
14-18 |
1300 |
|
19-30 |
1000 |
|
|
31-50 |
1000 |
|
|
Boys |
9-11 |
1000 |
|
12-18 |
1300 |
|
|
Men |
19-70 |
1000 |
|
>70 |
1300 |
|
| *Source: National Health and Medical Research Council. (2006) Executive Summary of Nutrient Reference Values for Australia and New Zealand Including Recommended Dietary Intakes. Commonwealth Department of Health and Aging, Australia, Ministry of Health, New Zealand. | ||
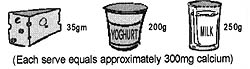
Dairy foods are the best source of calcium. They contain high levels of calcium which is easily absorbed by the body. Low fat varieties are available to reduce the risk of weight gain or raised cholesterol levels.
Canned fish with edible bones is also a good source of calcium. The calcium found in many other foods, including vegetables and nuts, is not efficiently absorbed into the body.
Post-menopausal women should have at least 1300mg of calcium each day (three glasses of milk or equivalent). Women who have difficulty consuming this amount should take a calcium supplement at night.
Although calcium does not prevent bone loss, it is important in the over-all prevention of osteoporosis when combined with exercise, oestrogen and other therapies.
Foods rich in calcium
Dairy foods:
- Milk, 1 cup: 300 mg
- Yoghurt, 200g 300 mg
- Cheddar cheese, 1 slice: 300 mg
- Cottage cheese, 200g: 190 mg
Fruit and Vegetables:
- Lemon, 1 only: 110 mg
- Dried figs, 1 only: 60 mg
- Broccoli, 100g: 70 mg
- Pumpkin, 100g: 40 mg
Fish:
- Sardines (with bones)100g: 300 mg
- Salmon (with bones) 100g: 300 mg
Soy Products:
- Calcium fortified soy milk 250 ml: 290 mg
- Soy or kidney beans, 70g: 70 mg
Miscellaneous:
- Almonds, 50g: 125 mg
- Ovaltine, 10g: 250 mg
- Pizza with cheese, 150g 240mg
- Quiche Lorraine, 150g 260mg
- Sesame seeds (black) 1 tbs: 200mg
Exercise
Regular weight bearing exercise including resistive exercise with weights increases bone mass at all ages, stimulates bone growth, and improves flexibility and coordination. Recommended activities are: walking, jogging, tennis, dancing for at least 30 minutes three to four times a week.
Other Measures
- Avoid cigarette smoking.
- Reduce alcohol and caffeine intake.
Can hormone replacement therapy help?
Oestrogen replacement at menopause prevents bone loss, but only as long as the therapy continues – that is, as long as the woman remains on HT.
When the woman stops taking oestrogen bone loss begins again. The dose of oestrogen required may be different for different women. All women should consider oestrogen to prevent bone loss after menopause, particularly those women who enter menopause with a low bone mineral density or with an early menopause.
Oestrogen replacement is often necessary to prevent bone loss in young women who do not ovulate regularly, such as may occur in anorexia and with polycystic ovaries. When oestrogen therapy is not appropriate other therapies may be prescribed.
How is osteoporosis diagnosed?
The most reliable way of diagnosing osteoporosis is by measurement of bone density. This is usually, and most reliably, done by the technique known as DEXA. DEXA uses X-ray technology, involves minimal radiation, is accurate, and can be used to monitor the effects of treatment and/or to monitor for disease progression as time passes.
What can be done for women with osteoporosis?
It is never too late to seek treatment. Treatment can halt bone loss and significantly reduce the risk of fractures.
HT is a very effective treatment for osteoporosis and is mostly prescribed when a woman has reduced bone density and menopausal symptoms.
Medications prescribed for women who have had a fracture include alendronate, etidronate, raloxifene, and calcitriol. All these treatments appear also to strengthen bones and prevent fractures, and they may improve bone density.
All these treatments appear also to strengthen bones and prevent fractures, and they may improve bone density.